To view (part 1) comments from the announcement click here
To view (part 2) comments from announcement click here
By Cecilia Nasmith/Today’s Northumberland
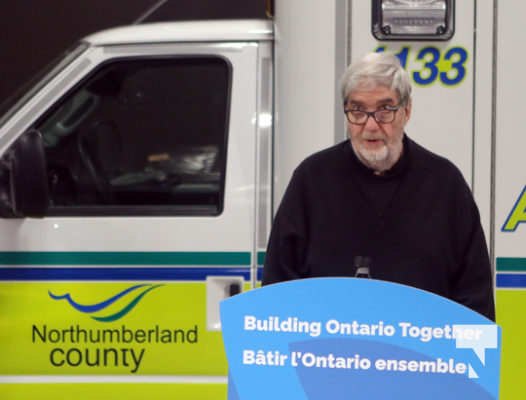
Months of consultations, applications, and even site visits from provincial officials reached a successful conclusion Friday at the Colborne Emergency Service base, as Deputy Premier and Minister of Health Christine Elliott delivered the good news.
The Northumberland community is one of the first to be recognized by the province as an Ontario Health Team – now to be known as Ontario Health Team-Northumberland.
This new integrated model of care depends on collaborations and communications to deliver a patient-centred model that provides an equitable and seamless continuum of care. Since the new model was announced, a number of local partners have pitched in to go through the process to win that designation.
Northumberland County chief administrative officer Jennifer Moore noted that the county has a long history of collaboration and building on partnerships, making it an ideal community for an OHT – and as the provider of paramedic services as well as a range of social services, the county has its own role to play.
“Boy, is it a special day to acknowledge and build upon the already-efficient partnerships, but also to take it one step further,” Northumberland-Peterborough South MPP David Piccini said.
“What’s unique is, we are seeing an opportunity to see health care that is fundamentally centred around the patient, and you all have the opportunity to design it.
“It’s a grassroots-up approach to health care that puts the patient first. The province is introducing this as the new model of care that brings together health-care providers to work as one team, and Northumberland is one of the first teams approved.”
“This is truly a significant day for the future of health care here in Colborne, but also a great day for the future of health care across Ontario,” Elliott said.
“We all know our health-care system is facing capacity pressure right now, and many of our patients and their families are getting lost in our health-care system. That is why our government committed to its citizens to create an integrated and sustainable health-care system focused on the needs of patients and families,” she said.
Elliott expanded on how OHTs will do a better job of supporting patients and families by connecting health-care providers to work as one single team to ensure a better patient outcome at every step of his or her health-care journey. For example, a hospital can work with home-care service providers to prepare for a patient’s eventual discharge by ensuring every service someone recovering at home would require.
The groundwork for this ideal model in Northumberland has been recognized by the province, Elliott said, “after a pretty arduous assessment procedure, involving a lot of collaboration, research and teamwork, and hundreds and hundreds – if not thousands – of hours of work.
“It’s an exciting time, as we finally break down the barriers that have kept providers from collaborating and communicating with each other to provide patient-centred care.”
Elliott listed the many partners who came together in Northumberland to create this team included patient and caregiver representatives and primary care providers, as well as representation from Alderville First Nation, both Northumberland hospital, community health centres, family health teams, long-term care, community-care support services, emergency medical services, hospice palliative care, housing and mental health.
The government’s focus has always been to end hallway medicine, Elliott said, listing the four pillars supporting this strategy.
First, keep people out of hospitals in the first place through prevention strategies and health promotion.
Second, ensure the right care is delivered at the right place. Hospitals are not always the right place for a patient to be, especially at a time when many are operating at 110% capacity.
Third, all facets of care must be integrated to improve patient flow.
Fourth, build capacity throughout the system by investing $27-billion over the next 10 years in hospital infrastructure and building long-term-care capacity.
“I congratulate you and thank the Ontario Health Team for the impressive work you have been doing,” she said.
“I know with all of you working together – and it’s going to take all of us working together as a team, we’re all in this together – I know we are going to be able to provide excellent-quality patient-centred care to everyone in Ontario, to give them the care they deserve .”
Northumberland Hills Hospital president and chief executive officer Linda Davis said she was delighted to represent her colleagues in the OHT endeavour in thanking the province.
“We believe each member of this county – patients, future patients, family members, care providers – will benefit from a more connected local health-care system that we are forming and launching today,” Davis said.
“Northumberland has learned first-hand that the most creative and sustainable thinking evolves when those most affected by the decision are part of making that decision. We have included a number of individuals, but truly I think we have been more than pleased to have all the partners come to the table, particularly our patient and caregiver representatives.”
Davis identified their patient and caregiver representatives as Kay Jackson and Scott McPherson. Though Jackson could not be present, McPherson was invited to say a few words.
“Kay and I have, from the beginning, felt equal and influential,” he said.
McPherson said he has occasionally had to leave the county for the health care he requires, but he appreciates those times he is able to receive what he needs in the community where his life and his friends are.
“There’s a great deal of enthusiasm, creativity and energy around this work, something beyond what we have ever experienced before,” Davis said.
“There’s much work still to do. Patients, caregivers and providers are frustrated by the disconnected system – which we could also call a loose collection of services.”
Davis outlined some particular initiatives which the local OHT hopes to implement with its own particular population in mind – a population that skews to the older side of the demographics and includes a significant rural complement.
Projects that will begin to be implemented in 2020 include the Volunteer Peer Support initiative, Community Paramedicine and Rural Outreach Clinics.
The first will see trained volunteers reaching out to those who require assistance in navigating the system. The second will leverage the skills of the county’s trained paramedics in the monitoring of patients. The third will bring health care out of established locations into rural areas for easier access to help reduce some barriers that now exist.
A fourth project team to be developed will focus on Digital Health.
The province is continuing to review applications for OHT status from communities across Ontario.
Just the night before Elliott’s announcement, Davis had reported at the Northumberland Hills Hospital board meeting on the latest site visit by Ministry of Health officials to the community on Nov. 15, where local members of the initiative explained proposed priority projects. They were also able to report to the ministry that more than 97% of local primary-care providers are on board with the new model, believed to be the highest for any OHT to date.
“The OHT is one of the more important health-care initiatives in the transformation of health care, and will ensure local patients receive the right care at the right place,” Piccini said.